
Sleep is important (we all know this) … but just how important is it?
Poor sleep is associated with increased depression, anxiety, systemic inflammation and decreased immune function.
For those with Restless Leg Syndrome, a lack of sleep is likely a nightly occurrence. It’s also the most dangerous side effect of this frustrating condition.
Worse yet, many suffer from Restless Leg Syndrome and don’t know it.
RLS can often be misdiagnosed as another sleep disorder, depression, poor circulation, arthritis, back problems and even growing pains in children.
If you have extreme fatigue, trouble falling or staying asleep, depression or anxiety, take the time to keep reading.
WHAT IS RESTLESS LEG SYNDROME?
Restless Leg Syndrome (RLS) is a neurological condition characterized by an uncomfortable feeling in the legs (most commonly). The unpleasant feeling causes an intense urge to move the lower extremity in order to find relief. The sensation is more prominent at night and is often described as “bugs crawling up the legs.”
The side effects of RLS are more concerning than the condition itself, and include:
Insomnia
Extreme daytime fatigue
Increased use of sleeping medications or alcohol to sleep
Increased use of stimulants in order to function
Increased stress (likely due to lack of sleep) and anxiety
Restless Leg Syndrome, also known as Willis-Ekbom Disease or WED, is most common in middle to older-age women, although anyone can experience it. The National Sleep Foundation estimates up to 10% of adults suffer from RLS.
 HOW IS RLS DIAGNOSED?
HOW IS RLS DIAGNOSED?
The International Restless Leg Syndrome Study Group requires the following clinical features to be present in order to confirm a diagnosis of RLS:
Strong urge to move the legs due to uncomfortable sensations in the leg(s)
Symptoms become worse during periods of rest or inactivity
Symptoms are partially or totally relieved by movement
Symptoms become worse in the evening or nighttime
Symptoms are not solely accounted for by another condition (i.e leg cramps, positional discomfort)
Perhaps the most important tool, though not always performed, is a test to determine your iron levels. The most accurate way to determine if iron deficiency plays a role in RLS is to measure ferritin. Ferritin is an iron binding protein in which low values (less than 50 ng/ml) indicate low iron storage in the brain (more on iron below).
IS RLS A GENETIC CONDITION?
First degree relatives are 3 to 6 times more likely to suffer from the condition and over 50 percent of affected individuals report having at least one immediate relative with the condition.
Studies suggest when children experience RLS (early onset) it is more likely due to genetics as opposed to onset later in life (after the age of 45). Several gene variations have been studied as possible contributors to RLS, including the following genomic regions: BTBD9, MAP2K5, MEIS1, PTPRD, SKOR1 and TOX3.
Risk allele BTBD9 is associated with RLS and decreased peripheral iron stores – a well-defined environmental factor in which the risk of RLS is about 9 times greater than the general populations.
A change in the BTBD9 gene is present in about 75% of patients who have RLS but also present in about 65% of patients who don’t have RLS…
The difference? Environmental factors.
It’s the environmental triggers in combination with the right genes that trigger Restless Leg Syndrome.
Genetics alone rarely tell the whole story (and that holds true for each of the autoimmune conditions we’ve covered).
TRIGGERS FOR RESTLESS LEG SYNDROME
Caffeine – Caffeine, most commonly found in coffee, tea, chocolate, and soda may aggravate the symptoms of RLS. For many, caffeine activates excitatory neurotransmitters and has an arousal effect on the central nervous system. Ultimately, it’s effects promotes motor activity and inhibits proper control of fine motor movements, worsening the symptoms of RLS.
Iron Deficiency – The most consistent finding and the strongest environmental risk factor associated with RLS is iron insufficiency. Studies suggest that restless leg syndrome is related to a deficiency of iron in certain parts of the brain despite normal levels in the blood. (See information on testing iron in the diagnosis section.)
Vitamin D Deficiency – One of the most common theories about the cause of RLS is impaired dopamine signaling, and vitamin D is now being researched for its role in this process. Several studies support the hypothesis that a deficiency of Vitamin D correlates with more frequent and more severe symptoms of RLS.
Diet – Vitamin B12 is a critical part of a healthy nervous system, helping to maintain and protect the myelin sheath around the nerves. Researchers are led to believe it could play a role in the onset and treatment of RLS, due to its central role in our nervous system and brain.
A study published in the Journal of Postgraduate Medicine found both iron and vitamin B12 deficiencies to be common and treatable cause of RLS.
The best dietary sources of Vitamin B12 come from beef liver, grass-fed beef and eggs. But in order to absorb Vitamin B12, we must have adequate stomach acid levels and a healthy gut.
Stress – Chronic stress can alter cortisol production and lead to nighttime cortisol release, which researchers have found to be correlated with RLS. Stress levels can also decrease dopamine in the brain – a neurotransmitter necessary for smooth muscle activity and movement. When dopamine is decreased in the brain, it may cause movement problems seen in Parkinson’s disease and RLS.
Pregnancy – The prevalence of RLS during pregnancy is two to three times higher than in the normal population. Hormonal changes and iron status are the two main factors that may contribute to RLS during pregnancy.
Researchers have discovered another piece to the puzzle in the onset of RLS – systemic inflammation.
 SYSTEMIC INFLAMMATION – THE CAUSE OF RESTLESS LEG SYNDROME?
SYSTEMIC INFLAMMATION – THE CAUSE OF RESTLESS LEG SYNDROME?
What if the cause of those frustrating leg twitches is something you can’t see or touch… and is rarely a diagnosis you’d receive at the doctor’s office?
We’re talking about systemic inflammation (inflammation relating to the whole body).
54 diseases, syndromes and conditions have been reported to cause and/or exacerbate RLS – all interconnected by inflammation.
The fact that 89% of RLS-associated conditions are associated with inflammation and/or immune changes have led researchers to develop 2 possible theories in the RLS – Inflammation connection:
Systemic inflammation can contribute to an iron deficiency in the brain:
Inflammation can lead to the production of IL-6, an inflammatory cytokine which can stimulate hepcidin production.
Hepcidin is the main hormone involved in the regulation of iron and increased levels can lead to decreased serum iron levels. The result? Decreased availability of iron to the brain.
Systemic inflammation can trigger autoimmune disorders associated with RLS.
RLS is associated with Multiple Sclerosis, Rheumatoid Arthritis, Sjögrens syndrome, Scleroderma, Celiac disease and Crohn’s disease – all autoimmune diseases plagued by systemic inflammation.
RLS is present in up to one third of MS cases and is also common in those with Crohn’s disease – a disease associated with iron deficiency, inflammation, and bacterial overgrowth. One study of 272 Crohn’s disease patients found 30% were affected by RLS.
The bottom line is this – we have to address the factors in our life that cause inflammation and the best place to start is a damaged gut.
A LEAKY GUT – THE MISSING LINK IN RESTLESS LEG SYNDROME?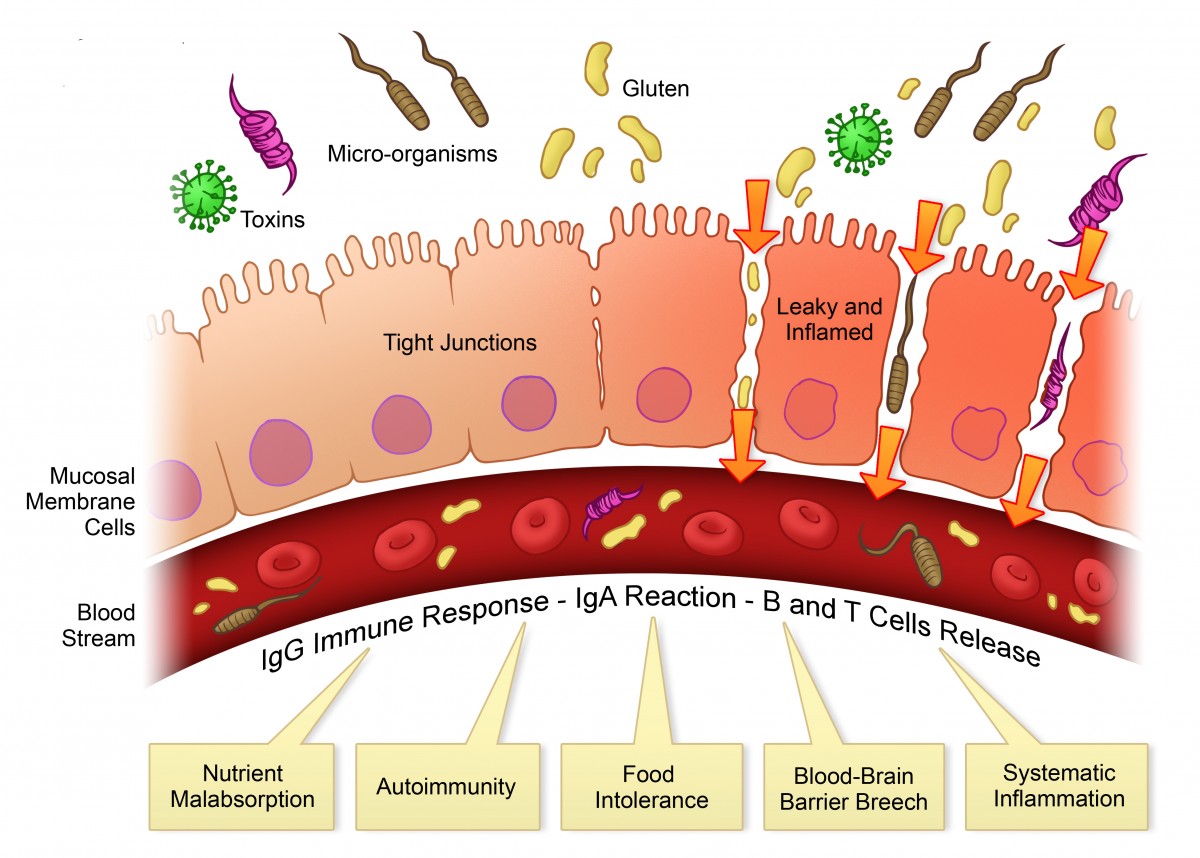
You might wonder what the gut has to do with that uncomfortable feeling in your legs.
A damaged or leaky gut is a breeding ground for inflammation – the very inflammation that can lead to RLS.
A leaky gut allows conditions like SIBO (small intestine bacterial overgrowth), and irritable bowel syndrome (IBS) to wreak havoc on the body and contribute to things like RLS.
One study found 69% of RLS patients had SIBO while 28% also suffered from IBS symptoms (i. e. gas, cramping, bloating, and changes in bowel habits).
SIBO can lead to systemic inflammation and autoimmune changes (which can result in the nerves being attacked in RLS) and SIBO induced inflammation can increase hepcidin (the main hormone responsible for regulating iron).
No matter which way we look at it, inflammation is the common denominator.
So, how do we stop the inflammation that can lead to Restless Leg Syndrome?
Considering the overwhelming amount of research on the topic of systemic inflammation and a leaky gut, your gut is too important to be ignored.
However, a large majority of the medical community has yet to accept the role of the gut in the fight against RLS.
 THE MEDICAL APPROACH TO TREATING RESTLESS LEG SYNDROME
THE MEDICAL APPROACH TO TREATING RESTLESS LEG SYNDROME
Dopaminergic agents are often the first line of treatment in RLS. These drugs work to increase dopamine in the brain and include Requip, levodopa, and Neupro to name a few.
Known for their short-term effectiveness, they come with a long-term effects.
Augmentation is the most common side effect of dopaminergic drugs and occurs when the symptoms of RLS become more severe, happen earlier in the day, and spread to other parts of the body (i.e arms).
It’s estimated that over 80% of patients receiving levodopa for RLS develop augmentation.
With augmentation, the brain sees the extra dopamine (via medication) as a signal to decrease its natural production. The result? Patients become increasingly dependent on the drugs for relief.
Compulsive behavior is also a common side effect.
A study including 100 people with RLS (all were treated with dopaminergic agents) revealed well over 50% engaged in some type of compulsive behavior (ie. pathological gambling and compulsive eating habits).
After reading this, you may be wondering if there is a better way to treat RLS than the use of these dangerous medications.
THE LEAKY GUT – AUTOIMMUNE CONNECTION
If you’ve been keeping up with the latest information in natural health, you already know it’s nearly impossible to ignore a leaky gut as part of the cause and solution to autoimmune conditions like RLS.
Alessio Fasano, M.D. has been on the forefront of recent autoimmune disease research and published a paper titled “Leaky Gut and Autoimmune Diseases.”
His findings present the idea that in order for an autoimmune disease to develop, 3 conditions must all exist together:
1. A genetic predisposition to autoimmunity (i.e. BTBD9 gene in RLS)
2. An exposure to the environmental trigger (i.e. Iron Deficiency)
3. Increased intestinal permeability (a.k.a. Leaky Gut Syndrome)
For those with Restless Leg Syndrome, healing the gut means getting to the root cause so you can stop chasing your symptoms.
Healing a leaky gut is one factor that’s in our control and it can be done step-by-step with the right plan.
HOW TO TURN OFF AUTOIMMUNE DISEASE
Overcoming Restless Leg Syndrome requires a multifaceted approach to heal the gut and decrease inflammation – and that is exactly what we’re here to help you do.
Hippocrates, the famous Greek physician, stated “all disease begins in the gut,” and some 2,000 years later Fasano and many other leading experts agree.
Ancient and current wisdom both suggest that powerful healing must begin in the gut.
 Jordan Reasoner is a health engineer and author. He was diagnosed with celiac disease in 2007 and almost gave up hope when a gluten-free diet didn’t work. Since then, he transformed his health using the SCD Diet and started SCDLifestyle.com to help others naturally heal stomach problems.
Jordan Reasoner is a health engineer and author. He was diagnosed with celiac disease in 2007 and almost gave up hope when a gluten-free diet didn’t work. Since then, he transformed his health using the SCD Diet and started SCDLifestyle.com to help others naturally heal stomach problems.






 Multiple studies show that there is an undeniable bond between Restless Legs Syndrome and anxiety & panic disorders.
Multiple studies show that there is an undeniable bond between Restless Legs Syndrome and anxiety & panic disorders.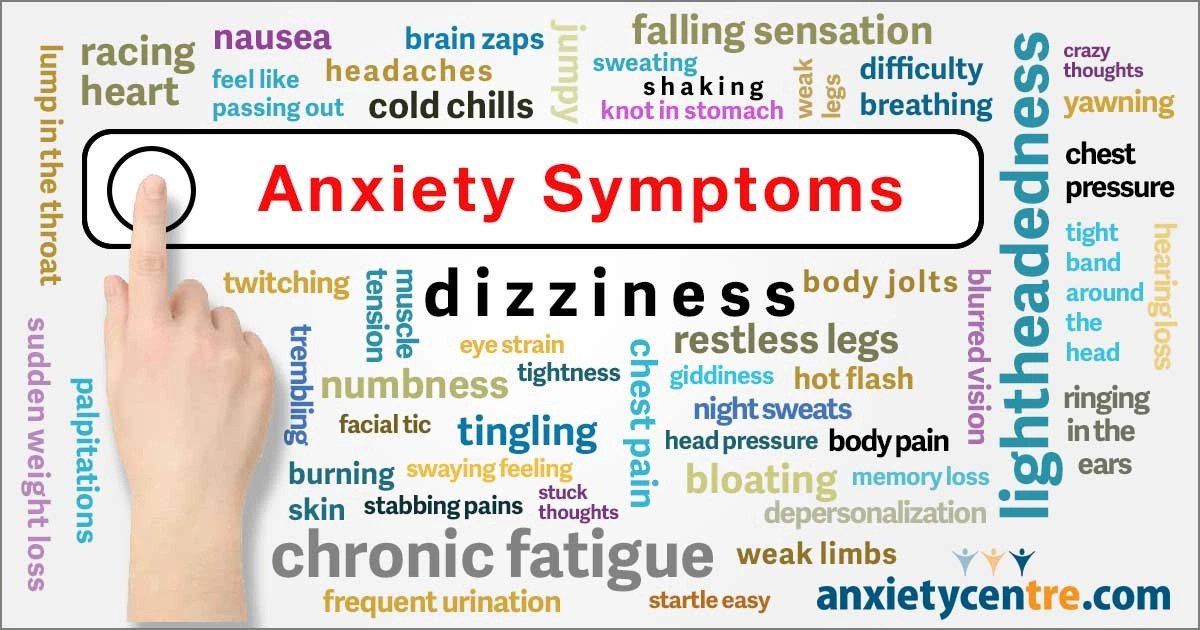
 CORRELATION OF ANXIETY AND DEPRESSION SYMPTOMS IN PATIENTS WITH RESTLESS LEGS SYNDROME: A POPULATION BASED SURVEY
CORRELATION OF ANXIETY AND DEPRESSION SYMPTOMS IN PATIENTS WITH RESTLESS LEGS SYNDROME: A POPULATION BASED SURVEY
 than in patients without RLS symptoms (54.3% in anxiety patients with RLS symptoms vs 23.8% in anxiety patients without RLS symptoms).”
than in patients without RLS symptoms (54.3% in anxiety patients with RLS symptoms vs 23.8% in anxiety patients without RLS symptoms).”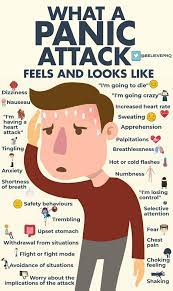 “Compared with non-RLS controls, patients with RLS are 5 times more likely to experience panic attacks or have comorbid panic disorder or generalized anxiety disorder.”
“Compared with non-RLS controls, patients with RLS are 5 times more likely to experience panic attacks or have comorbid panic disorder or generalized anxiety disorder.”
 Experiments with patients suggest brain stimulation may be a viable treatment
Experiments with patients suggest brain stimulation may be a viable treatment mechanism for RLS rests in the brain’s “move my legs” center and makes even more sense of the relief those with RLS experience when they get up and move them.
mechanism for RLS rests in the brain’s “move my legs” center and makes even more sense of the relief those with RLS experience when they get up and move them. “This basically means that inhibition is reduced or weakened in people with restless legs syndrome compared to people without the condition,” says Rachel Salas, M.D., associate professor of neurology at Johns Hopkins. “The reduced response means that the region of the brain controlling the legs shows increased cortical excitability in the motor cortex.”
“This basically means that inhibition is reduced or weakened in people with restless legs syndrome compared to people without the condition,” says Rachel Salas, M.D., associate professor of neurology at Johns Hopkins. “The reduced response means that the region of the brain controlling the legs shows increased cortical excitability in the motor cortex.” people with severe forms of the condition or at the long-interval paired pulses in the leg,” says Salas. “We are fortunate to have access to such individuals because the Johns Hopkins Sleep Center attracts people worldwide and many who have exhausted treatment options available elsewhere,” she adds.
people with severe forms of the condition or at the long-interval paired pulses in the leg,” says Salas. “We are fortunate to have access to such individuals because the Johns Hopkins Sleep Center attracts people worldwide and many who have exhausted treatment options available elsewhere,” she adds.

 HOW IS RLS DIAGNOSED?
HOW IS RLS DIAGNOSED?
 SYSTEMIC INFLAMMATION – THE CAUSE OF RESTLESS LEG SYNDROME?
SYSTEMIC INFLAMMATION – THE CAUSE OF RESTLESS LEG SYNDROME?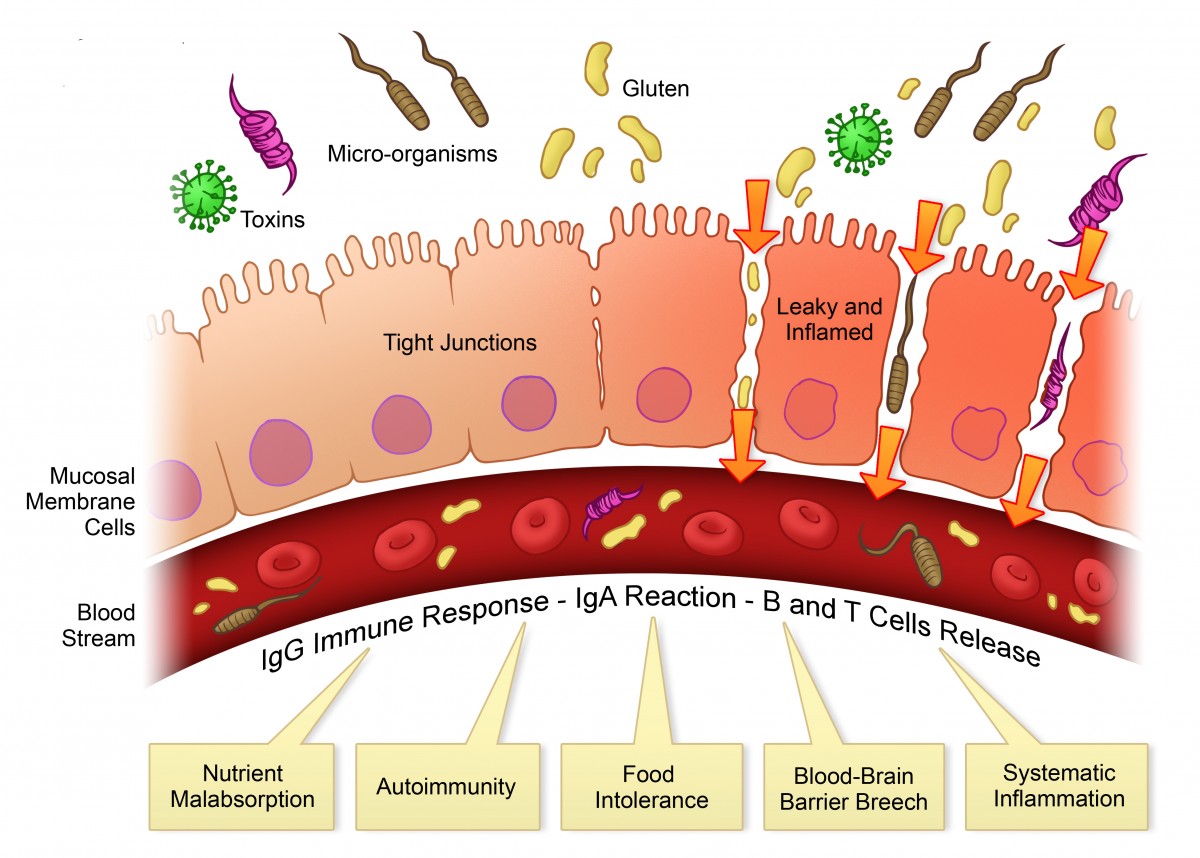
 THE MEDICAL APPROACH TO TREATING RESTLESS LEG SYNDROME
THE MEDICAL APPROACH TO TREATING RESTLESS LEG SYNDROME
 Jordan Reasoner is a health engineer and author. He was diagnosed with celiac disease in 2007 and almost gave up hope when a gluten-free diet didn’t work. Since then, he transformed his health using the SCD Diet and started SCDLifestyle.com to help others naturally heal stomach problems.
Jordan Reasoner is a health engineer and author. He was diagnosed with celiac disease in 2007 and almost gave up hope when a gluten-free diet didn’t work. Since then, he transformed his health using the SCD Diet and started SCDLifestyle.com to help others naturally heal stomach problems. Below is another study that supports the idea of inflammation being at the core of Restless Legs Syndrome.
Below is another study that supports the idea of inflammation being at the core of Restless Legs Syndrome.